As humans live longer, they’re at increased risk of developing devastating NEURODEGENERATIVE diseases, such as Alzheimer’s—in a treatment landscape with few options and little hope. At Scripps Research, scientists are closer than ever to understanding how these diseases harm the brain and identifying possible drugs to stop them.
As a neuroscientist, Hollis Cline, PhD, was well aware of the predictions that the number of people living with dementia worldwide was expected to nearly double every 20 years—reaching 78 million in 2030 and 139 million in 2050.
Still, she didn’t expect to witness dementia’s excruciating progression in her own parents. “It’s a particularly mean disease,” says Cline, Hahn Professor of Neuroscience and director of the Dorris Neuroscience Center. “It steals people’s identity, and it’s heartbreaking for the people around them to watch their decline.” People with dementia typically experience memory loss and confusion and, over time, stop recognizing their loved ones. They slowly lose their ability to speak, bathe, dress and feed themselves.
In addition to the emotional and physical toll on families, the economic costs of long-term care and unpaid caregiving are estimated to exceed $300 billion annually in the United States alone.
Making the experience even more painful for Cline and her family was the fact there were not many treatments available. Unlike many other areas of medicine, there have been few breakthroughs in the field of neurodegenerative diseases, a broad category of debilitating conditions, including Alzheimer’s, Parkinson’s, Huntington’s and multiple sclerosis, that are caused when nerve cells lose function and die. The published failure rate for drugs for major degenerative disorders is more than 98 percent. And even though the U.S. Food and Drug Administration (FDA) made headlines in 2021 for the accelerated approval of the Alzheimer’s drug aducanumab (sold under the name Aduhelm), there are widespread doubts about whether it offers a tangible benefit to patients. And the Centers for Medicare & Medicaid Services has limited its coverage to those enrolled in clinical trials.
Despite such odds, scientists at Scripps Research are leading a rare wave of progress. Cline and other scientists at the institute are rapidly deciphering the underlying causes of neurodegenerative diseases and in the process uncovering new possibilities for treating them.

“The brain is the great unexplored area. It’s the ‘Star Trek’ of biology. We’re still in the infancy of drug discovery, but we’ve discovered targets that were once thought to be undruggable. This is amazing progress.”
— Stuart Lipton, MD, PhD
Over the last two decades, Scripps Research scientists have ushered in seven FDA-approved drugs that target neurodegeneration. For example, the team of Hugh Rosen, MD, PhD, and Ed Roberts, PhD, invented ozanimod (Zeposia) for multiple sclerosis. Jeff Kelly, PhD, was responsible for discovering tafamidis (sold under the names Vyndaqel and Vyndamax) for cardiomyopathy and familial amyloid polyneuropathy—a disease that progresses to dementia. In 2003, the agency approved Stuart Lipton’s memantine (sold under the brand names Namenda, NamendaXR and Namzaric) to alleviate symptoms of moderate-to-severe Alzheimer’s disease, and the drug is often used off-label for other forms of dementia, such as vascular dementia resulting from multiple strokes. The drug is also used off-label for Lewy body dementia, a form of dementia associated with Parkinson’s disease, based on positive early clinical trials. More recently, a spinout company founded by Lipton, MD, PhD, also received FDA approval for an additional drug, amantadine (GoCovri), to treat motor symptoms of Parkinson’s disease.
Building on this success and the institute’s strengths in studying the underlying biological causes of neurodegeneration, last year Scripps Research launched the Neurodegeneration New Medicines Center to attract and support early-career faculty with novel ideas and funding sources.
The idea is to create a hub of research that uncovers critical insights of brain pathways, says Lipton, who co-founded the center with Kelly. That emphasis on basic science combined with Scripps Research’s commitment to translational research—through its drug discovery arm, Calibr—provides unique opportunities to find therapeutic applications.
For example, the team is growing cerebral organoids—also known as “mini brains”—in a dish that are generated from a patient’s stem cells. Candidate drugs are being tested on this human model system, paving the way for personalized treatments. “By pharmacologically reinforcing resilience pathways that are present in young brains, we hope to be able to stave off these diseases for many years,” says Lipton, who is the Step Family Foundation Endowed Chair, as well as a professor in the departments of Molecular Medicine and Neuroscience and a practicing clinical neurologist.
To jumpstart the New Medicines Center, he recently received a $5.3 million leadership award from the National Institute on Aging (NIA) at the National Institutes of Health to foster drug development at Scripps Research for Alzheimer’s disease and related dementias. “We have some amazing scientists here at Scripps Research at the forefront of this work,” he says.
Finding a new approach to an old problem
For Cline, witnessing her parents’ experience with dementia convinced her to change her research focus. During the first 30 years of her career, she studied the early development of the brain. Yet five years ago, feeling frustrated by the lack of treatment options for her parents, she decided to learn more about how the brain ages. “As a field, we need to explore more broadly the causes of dementia and how to use that knowledge to find new therapies,” she says.

“This early preclinical work may identify proteins that protect against cognitive loss. We know it’s a long path to get to a drug, but we’re creating the foundation. We know there’s an entire landscape of potential molecular interactions that maintain healthy synapses, and any of these proteins could be a drug target.”
— Hollis Cline, PhD
Cline was eager to take advantage of new technologies that could compare protein changes in specific cells in healthy brains and those ravaged by dementia—given that Alzheimer’s patients have fewer synaptic connections, which is how brain cells talk to each other. “The idea was to use these new tools for studying brain proteins in the context of aging with the hopes it would reveal something new for the field,” she says.
The professional pivot paid off. Last year, Cline’s lab was awarded a $1.3 million grant from the NIA in collaboration with Scripps Research neuronal connectivity expert Anton Maximov, PhD, and mass spectrometry expert John Yates, PhD, to look at the chemical changes of proteins over time in normal aging and in a mouse model of Alzheimer’s disease. The team will then test whether changing the protein expression to resemble the levels found in healthy brains would stop or slow down the loss of synapses.
“This early preclinical work may identify proteins that protect against cognitive loss,” Cline says. “We know it’s a long path to get to a drug, but we’re creating the foundation. We know there’s an entire landscape of potential molecular interactions that maintain healthy synapses, and any of these proteins could be a drug target.”
“Over the last 30 years, we’ve learned a lot about basic neurodegenerative disease pathobiology, and I predict that in the next 10 to 15 years these learnings will be translated into several new medicines available at the pharmacy.”
— Jeff Kelly, PhD
Why progress has been so elusive
Why have breakthroughs been so few and far between? And why is the history of neurodegenerative drug testing littered with hundreds of failed trials? For starters, studying the brain has been notoriously challenging. There are practical reasons; for example, researchers have had to find chemical tricks to bypass the blood-brain barrier and test drugs directly in the brain, and it’s hard to know if a drug could prevent the onset of dementia because they often only have access to symptomatic patients after they’ve been diagnosed.
But the bigger issue is whether researchers are focused on the right mechanisms to reduce dementia by treating the brain. For decades, scientists have embraced what’s known in the field as the “amyloid hypothesis.” That’s the idea that dementia is caused by the abnormal buildup of a particular misfolded proteins structure known as an amyloid fibril, which can form plaques that may impair normal cell functioning. When Kelly’s team discovered tafamidis, which was FDA-approved in 2019, for example, they found a medicine that reduced the entire process of aggregation from newly biosynthesized transthyretin. The formation of many non-native transthyretin structures, including amyloid fibrils, was blocked. This strategy slowed the progression of polyneuropathy, the malfunctioning of peripheral nerves throughout the body, and progression of cardiomyopathy, a condition that damages heart and neuropathy muscle. Tafamidis lowered the risk of death by 30 percent, notably without clearing the amyloid fibrils already present. And treatment with the drug seems to delay the onset of dementia so far, which eventually afflicts polyneuropathy patients.
In contrast, nearly all the strategies to treat Alzheimer’s disease studied in patients to date have sought to clear the amyloid fibrils already present, and not to prevent other non-native structures arising from the misfolding of newly synthesized amyloid-beta or tau protein. So far this strategy has failed to improve dementia. Thus, there isn’t clear evidence that clearing amyloid plaques improves Alzheimer’s disease symptoms.
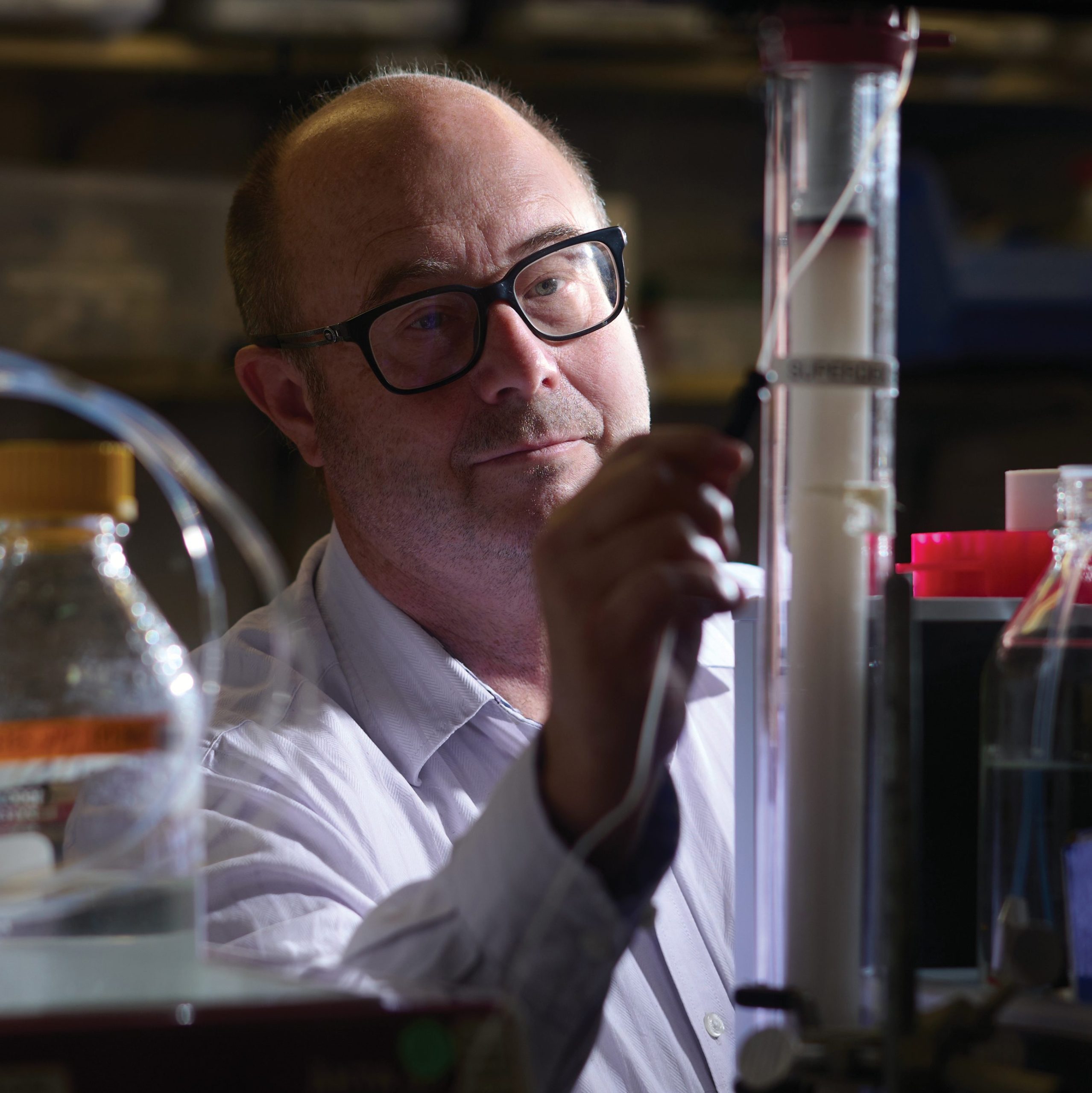
To complement the successful drugs that slow the progression of neurodegeneration by preventing newly synthesized protein from misfolding and aggregating, Kelly, who is the Lita Annenberg Hazen Professor of Chemistry, says, “Half my lab is working on new ways to degrade non-native proteins to keep their concentration low.” He adds that it may not be enough to stop the newly synthesized proteins from aggregating; the next frontier will involve understanding how to accelerate the natural processes in which the brain gets rid of these misshapen proteins believed to be linked to neurodegeneration. So far, in collaboration with Calibr, Kelly’s team has identified 80 “compounds of interest” and is focusing on four of them to enhance the lysosomal degradation of misshapen proteins.
“Over the last 30 years, we’ve learned a lot about basic neurodegenerative disease pathobiology, and I predict that in the next 10 to 15 years these learnings will be translated into several new medicines available at the pharmacy,” says Kelly.
Clues from rare disease
Another approach is unlocking whether specific mechanisms in rare fatal brain conditions called prion diseases could lead to understandings about the broader category of neurodegenerative diseases.
Scripps Research neuroscientist Sandra Encalada, PhD, is investigating a pattern of toxicity long observed in the brains of patients of nearly every neurodegenerative disease, from Alzheimer’s to Parkinson’s to Huntington’s. The shape of brain cells normally features a cluster of long, tube-like axons that jut out from one end of the cell body and are critical in the formation of memories.
During the early stages of these diseases, researchers noticed that bulges resembling trapped water in the ballooning knots of a garden hose had already started to form along these long axons. “The axons are impaired and more vulnerable than the rest of the cell and start dying off before the whole neuron does,” says Encalada, who is the Arlene and Arnold Goldstein Associate Professor in Scripps Research’s Department of Molecular Medicine and Dorris Neuroscience Center.
That association gave Encalada an important clue about where in the brain to pinpoint her research. She hoped that focusing on the mechanisms of prion diseases would provide a useful model to study other degenerative diseases. “What we learn from prion diseases could help us understand what causes failures in Alzheimer’s and other dementias,” she says. Encalada wanted to learn more about how prion proteins that fold incorrectly accumulate in these bulges and cause axons to prematurely die off and hurt people’s cognitive and motor functioning.

“Understanding the basic biology was key. Knowing the mechanisms of the cellular pathway that generates the bulges informed us which pharmacological mechanisms could stop those processes from occurring.”
— Sandra Encalada, PhD
Encalada’s lab recently received a $4.1 million grant from the NIA to study how these toxic bulges impair cellular functioning in patients suffering from inherited and transmitted forms of prion disease. In an ongoing mouse study, her team is aiming to illustrate the concept by testing the effect of a mutated prion protein that folds incorrectly in humans. Mutations in the prion protein in humans cause such bulges resulting in major insomnia and rapid cognitive decline. Although rodents have circadian rhythms like humans, they’re nocturnal and sleep when we’re awake. In collaborative studies with the lab of Michael Petrascheck, PhD, at Scripps Research, just as the researchers predicted, the mice who received mutated prion proteins slept less and remained active most of the day.
Now Encalada’s team is attempting to reverse the effect. They introduced a second genetically-modulated protein that targeted the prion protein’s cellular pathways and appeared to reduce the bulges in the brains of mice. The researchers are awaiting the results to see if the same strategy will reduce the rodents’ insomnia.
Collaboration among Scripps Research’s scientists is making another potential breakthrough possible: Encalada is testing the drug candidates that enhance breakdown of misshapen proteins identified in Kelly’s lab, which potently reduce bulges in neurons grown in petri dishes. Her lab is now exploring whether these drug candidates can also relieve the insomnia in her mouse models of prion disease. “Understanding the basic biology was key,” she says. “Knowing the mechanisms of the cellular pathway that generates the bulges informed us which pharmacological mechanisms could stop those processes from occurring.”
Encalada, Kelly and Petrascheck are now studying whether similar mechanisms and therapeutic strategies are also at play in Alzheimer’s disease. Such insights could potentially pave the way to finding more effective drugs for the neurodegenerative disorders that affect broader swathes of the population; at least 50 million people globally are estimated to be living with Alzheimer’s, and 10 million suffer from Parkinson’s, for example.
Scripps Research scientists will use understandings about misfolded protein pathways to tackle Parkinson’s and Huntington’s diseases, amyotrophic lateral sclerosis (also known as Lou Gehrig’s disease) and autism spectrum disorder.
“The brain is the great unexplored area. It’s the ‘Star Trek’ of biology,” says Lipton, whose team is studying the abnormal hyper-electrical activity that occurs in the brains of patients with Alzheimer’s and autism and designing drugs that rebalance it. “We’re still in the infancy of drug discovery, but we’ve discovered targets that were once thought to be undruggable. This is amazing progress.”

On the hunt for a new class of MS drug
Multiple sclerosis (MS) is the most common degenerative disease of the central nervous system in young adults, leading to loss of balance and vision, fatigue, cognitive difficulties and muscle stiffness for nearly one million people in the United States. It’s caused when the immune system destroys the protective covering of the nerves—known as the myelin sheath—and disrupts communication between the brain and body.
Yet research to find a drug has long been frustrating. Although researchers have made progress in developing several therapies that were recently approved by the FDA, the drugs only work in the short term, and patients’ symptoms eventually return. A challenge has been figuring out how to make cells repair the nerve covering—a process called remyelination that’s necessary for remission.
To answer that question, Scripps Research chemical biologist Luke Lairson, PhD, was especially curious about patients who had a relapsing form of the disease. He wanted to know why cells sometimes repaired the myelin sheath and enabled the patients to improve—only to stop functioning and allowing the disease to worsen. That began his quest to see if he could develop a regenerative drug that would program stem cells to be myelin fixers.
In collaboration with Calibr, Scripps Research’s drug discovery arm, Lairson’s team screened a million compounds on primary stem cells from rat optic nerves and found a class of drugs known as M1 muscarinic receptor antagonists that jumpstarts the repair process in rodent models. One drug was tested in a phase 2 clinical trial in MS patients at the University of California, San Francisco, and found to induce remyelination. Yet the problem is that humans would likely have to take four times what they could tolerate to experience the optimal efficiency, says Lairson, associate professor in the Department of Chemistry. His team is now focusing on three other candidates that ideally could be administered at lower doses.
The next step is to try them in mice with the help of a $1.5 million grant from the California Institute for Regenerative Medicine. “I hope that understanding how these compounds work will lead to highly effective therapies for multiple sclerosis and other de-myelination diseases,” says Lairson.