One morning in July 2020, Julia Moore Vogel was sipping a cup of peppermint tea when she noticed something strange. She couldn’t taste the strong flavor of the tea she was drinking.
Knowing that loss of taste was a common symptom of COVID-19, she immediately suspected the worst. She contacted her healthcare provider who assured her that as a young, healthy person, the loss of taste might be her only symptom and she would be fine in no time.
That, unfortunately, didn’t end up being the case. The acute phase of her illness progressed steadily. She began to have severe trouble breathing, to the point where she went to bed at night wondering if she would wake up in the morning. She drafted a will.
The transition out of the acute phase was slow. Her initial symptom of severe shortness of breath was replaced by persistent brain fog, daily headaches and chest pain caused by inflammation in different chest joints. Over the next six months, small every day tasks like taking a shower left her exhausted. Now, almost a year and a half after initially contracting COVID-19, she still suffers from intense fatigue and headaches.
“As a long COVID patient, one of the most jarring aspects of this disease was going to see multiple doctors and having them confess they really don’t know how to treat this,” Moore Vogel says.
The scale of long COVID disease burden is staggering. It is estimated that 10 to 30 percent of COVID-19 patients develop long COVID, with over 20 million individuals in the United States suffering from its debilitating effects. While Moore Vogel considers her own symptoms to be on the minor end, individual symptoms vary dramatically from neurological symptoms and chronic pain to inflammation and swelling; many patients are bedbound.
Empowering patients with data from wearables
Her work at the Scripps Research Translational Institute gives Moore Vogel unique perspective on how medical interventions and treatments are achieved. She directs the Participant Center for the All of Us Research Program, an NIH collaboration to build the largest, most diverse health database in history. Her team is tasked with enrolling participants from across the country as well as integrating mobile health technologies into the research program.
“From the beginning of my long COVID journey, I was wondering how I could contribute to the research space, either as a study participant or eventually leading some research of my own,” says Moore Vogel.
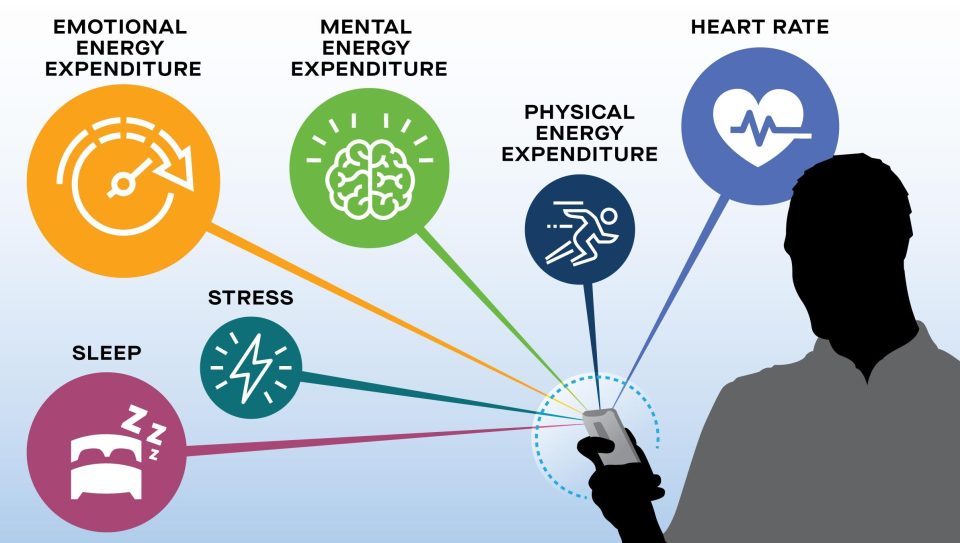
Through the Body Politic COVID-19 support group, Moore Vogel learned of something called pacing, which seemed to be helping many of her fellow long haulers manage their symptoms. Many patients had noted that their symptoms tended to get worse if they exerted themselves. By conserving the amount of physical, mental, and emotional energy a person used on a given day, they could avoid exacerbating their symptoms.
With expertise in digital health technologies, Moore Vogel began to monitor her own physiological metrics through a wrist-worn activity tracker. She quickly saw that she was able to better control her symptoms when she could track her own sleep, activity and stress levels, as well as her heart rate variability.
“I often didn’t realize I was overdoing things until two days later when I would have an increase in symptoms,” says Moore Vogel. “The activity tracker can quantify how much energy I use and help me avoid overexerting myself.”
The Long COVID Wearable Study
Her personal experience, combined with the experience of other long COVID patients, using a wearable device to manage symptoms inspired Moore Vogel to design a research study at Scripps Research that seeks to teach participants how to pace themselves to avoid overexertion. She hopes to be able to determine whether a wearable device can help people avoid relapses and potentially even provide long-term improvement in symptoms.
The Long COVID Wearable Study seeks to enroll 1,000 long COVID patients nationwide in a year-long research study.
“I’m really hopeful that this study can provide scientific evidence to reinforce what we’ve seen anecdotally in the community,” Moore Vogel says.
When discussing the future, Moore Vogel emphasizes the need for more awareness about long COVID.
“A lot of people think that either you’re hospitalized, you die or you’re a hundred percent fine. But there’s a distinct possibility of a lifelong, as far as we know at this point, disability that should really factor into people’s risk calculations,” she says.