As it turns out, our metabolisms have been misunderstood for decades. These Scripps Research scientists are changing the way we think about metabolic disorders, weight control and eating habits—paving the way for new drugs to treat some of the most serious health conditions our world faces today.
You’ve probably heard it before: “I have a fast metabolism.” Or maybe: “My metabolism has really slowed down.” But what does this frequently used term in science, health and medicine truly mean?
“Metabolism” is the process of how we convert our food into energy. It sounds simple—and for many scientists, it was simple. The prevailing thought was that you could easily influence it by changing what you ate, how much you exercised or the amount of muscle you built.
Yet scientists at Scripps Research are finding that our metabolisms are much more intricate than anyone previously imagined.
Our sleep cycles impact it. So do our environments, nerves, hormones, genes, and other interconnected mechanisms and cellular pathways that Scripps Research experts are now beginning to uncover. These insights are already shaping new therapeutics and interventions for controlling your weight and keeping your metabolism running at peak performance. This emerging research also comes at a critical time—roughly one in three adults in the United States has metabolic syndrome, a group of conditions that raises a person’s risk of heart disease, type 2 diabetes, stroke and other serious health complications.
Meet the Scripps Research leaders who are fueling a new era in metabolism research and drug development—with the intent to help improve metabolic health across the nation and globe.

SLEEP
How our sleep cycles affect how we burn fat, exercise and metabolize medicine
Katja Lamia, PhD
Associate Professor of Molecular Medicine
Before becoming a Scripps Research scientist, Katja Lamia got a powerful lesson on the effect our internal body “clocks” have on our health and wellbeing while working a student job in college. A few times a month, she was on security detail for the school’s dorms and stadium from 10 p.m. to 6 a.m. Predictably, she felt terrible the following few days as she tried to adjust back to a normal schedule.
It was an experience she never forgot as she focused her career on researching how altering our routines—even by just a few hours—can affect our bodies in surprising ways. Lamia is an expert in circadian rhythms: the body’s internal “clocks” that regulate our sleep and wake cycles. “We know there’s a circadian clock in the brain that drives when you are sleepy and when you are active, but we don’t fully understand how clocks in other parts of the body regulate other processes,” she says.
For example, during her PhD research, she had observed in mice that the time they received insulin injections determined the rate at which their cells took in blood sugar for energy. During her postdoc, she discovered in mice models that the liver has a clock that normally tries to predict the time of day when you’re not eating and increases the production and secretion of glucose, the body’s main source of energy. That finding is important support for the popular trend of “time-restricted eating” that’s believed to fine-tune your insulin sensitivity and improve weight control.
By the time she arrived at Scripps Research in 2010, Lamia wanted to dive deeper into the mysteries of the circadian clock in the hopes they could eventually help shift workers who chronically disturbed their physiology with often erratic work and sleep schedules. “I wanted to know more about why they were at increased risk of metabolic disease and cancer,” she says.
Among other findings, her lab has decoded how circadian clocks influence exercise performance and drug metabolism. Specifically, the proteins called CRY1 and CRY2 that regulate metabolism by suppressing a transcription factor (the process of converting DNA into RNA) are activated depending on the time of day. This mechanism plays a role in determining how and when you use fat and sugar for energy and explains why people usually can run faster later in the day. (Olympic records are usually set in the afternoon or evening.)
Lamia says that insight is helping researchers understand more about how we metabolize drugs at different hours of the day. She’s currently investigating the links between dosage timing and the response to metformin, one of the world’s most widely prescribed type 2 diabetes drugs. “Our results suggest that if you take the drug in the afternoon, it will have a different effect than if you take it in the morning,” says Lamia. “By understanding how something works, we can improve upon it. And small improvements could have a big impact.” That’s true for people who work during the wee hours of the morning or people who earn their living during daylight.

ENVIRONMENT
Deciphering metabolism clues from worms

Supriya Srinivasan, PhD
Associate Professor of Neuroscience
It’s a situation that’s frustrated many a dieter who has cut calories but still struggles to shed pounds: Does what you eat determine how much you weigh? Supriya Srinivasan was also intrigued by this question. “There’s a conundrum in the field about whether the brain regulates the body’s metabolism directly or indirectly by controlling food intake,” she says. “That’s the question that got me going because it’s unresolved.”
Srinivasan, an expert in gut-brain communication, hypothesized that a mysterious mix of environment and genetics influences the hormones that play a role in regulating body weight, yet those associations have been notoriously difficult to investigate in a complex system like the human body. So, Srinivasan came up with an innovative approach: search for the clues in roundworms. In scientific research, the tiny worm (called C. elegans) has become an increasingly popular model in which to find genes with similar functions in humans because more than 60% of the genomes of worms and humans have shared ancestry.
In their research, Srinivasan’s team uncovered a series of brain circuits the worms use to detect food, oxygen and population density in the environment, which helps determine how much there is to eat. It’s a strategy to make sure their bodies adapt to the amount of food available and burn the right amount of energy. “We found that the circuits in the brain that regulate feeding and the ones that regulate fat are totally different from one another,” she says.
Srinivasan’s team was also surprised to learn how much of this process took place in the gut. They found a peptide (a short chain of amino acids) that’s released by the brain and acts in the intestine to determine how much fat is metabolized. If there’s too much of the peptide, the mitochondria (cellular powerhouses that burn fat) in the intestinal cells get overwhelmed and set off a stress response that puts the brakes on the fat-burning process. “This shows how complex the relationship between fat metabolism
and the mitochondrial stress response is,” she says.
The discovery of those pathways suggests our brains may be using sophisticated strategies every day to calculate how to utilize the fat coming into the intestine. “There’s a lot of input from the sensory environment that goes into regulating metabolism. I couldn’t have imagined it, but that’s the beauty of science,” she says.
So, how might these insights apply to humans someday? Now that the worms have given Srinivasan a genetic map, she hopes to eventually find a drug target in humans. “Our goal is to uncover new features of fat metabolism,” she says.
Precision nutrition goes digital
Edward Ramos, PhD
Director, Digital Clinical Trials
The old saying goes: “An apple a day keeps the doctor away”—and, generally speaking, it’s good advice. The problem is that when it comes to nutrition and metabolism, general guidelines may overlook our individual biology, history and environment.
That’s where the emerging field of precision nutrition comes in. Scientists are combining data from our DNA, microbiome and metabolic responses to paint a more complete picture of how our unique traits, environment and lifestyle impact our overall health. These new insights are helping tailor metabolic disease prevention and treatment plans with increasing precision.
Simultaneously, the rise in wireless sensor technologies, from continuous glucose monitors to smartwatches that track a range of physiological metrics, enables scientists to give us a more in-depth view of how our bodies respond to the food we eat.
Edward Ramos, at the Scripps Research Digital Trials Center, is leading an innovative study into this vital area of research. The PRediction Of Glycemic RESponse Study (PROGRESS) is using a multitude of digital tools to investigate metabolic health and its connection to diseases like type 2 diabetes.
“PROGRESS is the most ambitious at-home digital clinical trial we’ve undertaken so far,” Ramos says. Study participants share health data—through smartphone apps, electronic health records, self-administered bio-sample collections and various sensors and monitors—to help scientists better understand how different people process nutrients.
“This assortment of data will not only provide insights into metabolic health, but the site-less, participant-centric study model, enabled through the use of digital technologies, allows us to pay particular attention to engaging individuals historically underrepresented in biomedical research by reaching them where they are,” says Ramos.
To learn more about PROGRESS, visit progress.scripps.edu

COMMUNICATION
Eavesdropping on conversations between your brain and fat stores
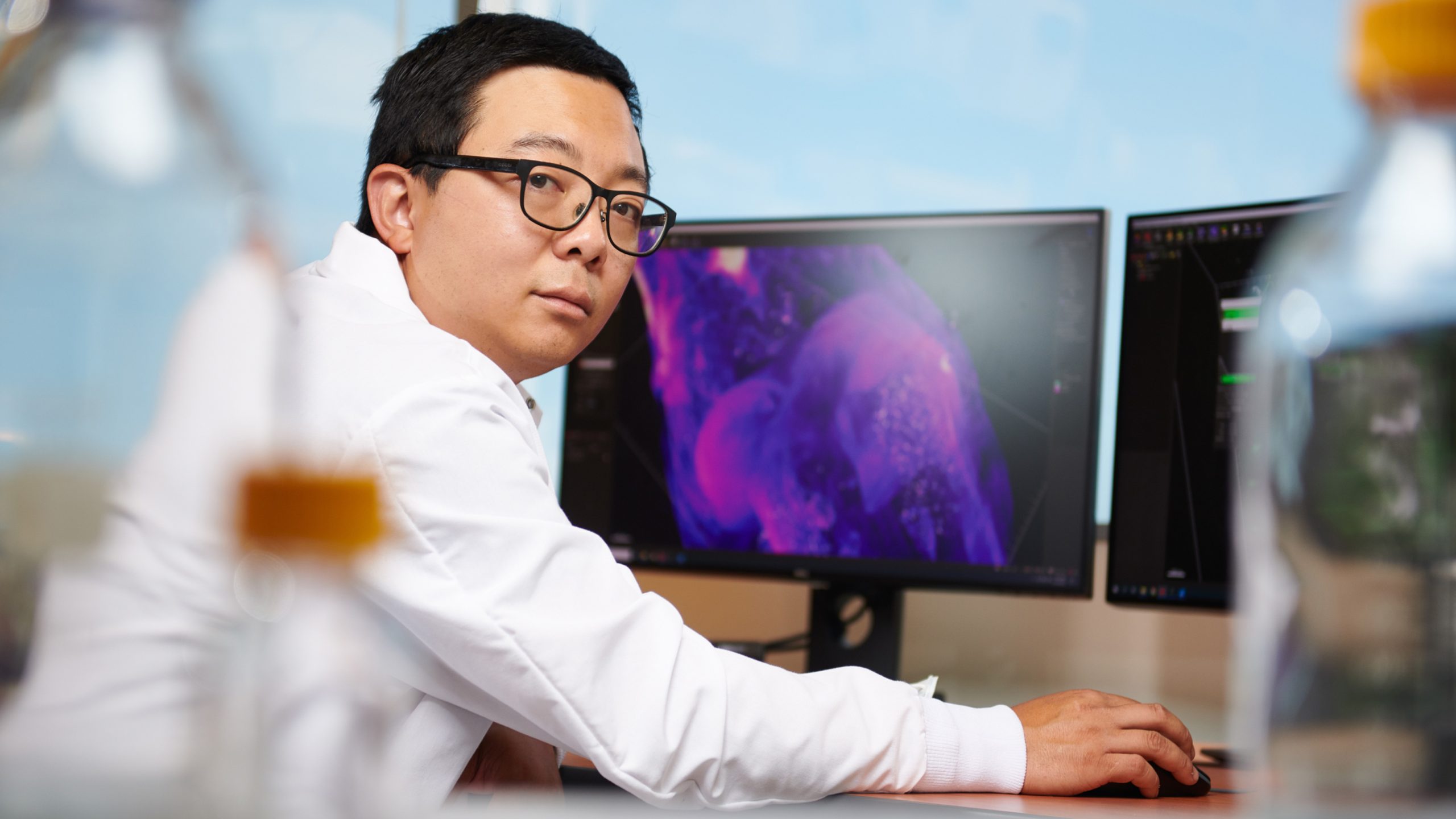
Li Ye, PhD
The Abide-Vividion Chair in Chemistry and Chemical Biology, Associate Professor of Neuroscience
Scripps Research neuroscientist Li Ye has long been frustrated by the simplistic explanation that the brain was solely in charge of telling the body how much fat to burn. Rather, he wanted to investigate if our fat talks back to our brain—and if so, how the tissue sends those messages. It’s a well-established fact that fat communicates by secreting hormones into the blood, but Ye and his team developed a specialized microscope that made it possible to detect new sensory neurons that emanate from the spinal cord to the fat tissue. “We found an actual hardwired nerve that gives the brain real-time feedback on whether it should increase or decrease the rate of fat-burning in terms of how much you should eat,” says Ye. The advantage, he says, is that the nerve sends the message quickly and can tell the brain where in the body the burning is going on.
Ye explains how the two-way dialogue works hypothetically: Let’s say you didn’t eat dinner last night, so your body knows it needs to release energy from fat. But your body also needs to know how fast to release it so it doesn’t run out. And that’s where this nerve might play an important role. “It’s like you know you need water, so you turn on your faucet, and you need to know how much water is actually flowing out in a given time,” he says. “In theory, you can turn it up or down depending on what you need.”
Now that Ye’s team has identified this fat communication pathway, they’re working on developing a new method to decipher exactly what the fat is saying. To accomplish this, they are experimenting with a combination of genetics, optical engineering and electrical recordings. “We’ll keep trying one by one. Then if we can understand its special signal, we’ll be closer to understanding how to block it and burn more fat,” he says.
Naturally occurring metabolite converts ‘bad’ fat to ‘good’ fat
In a study from Metabolites published in August 2022, Scripps Research and Calibr researchers used novel drug discovery technologies to uncover a metabolite that converts white fat cells (“bad” fat) to brown fat cells (“good” fat).
“With our technology, we can pull out endogenous metabolites—meaning the ones that the body makes on its own—that can have the same impact as a toxic drug with less side effects,” says co-senior author Gary Siuzdak, senior scientific director of the Scripps Center for Metabolomics and professor of chemistry, molecular and computational biology at Scripps Research.
Metabolic diseases are often caused by an imbalance in energy homeostasis, which is why certain therapeutic approaches have centered around converting certain adipocytes, or fat cells, from white fat cells into brown fat cells. White adipocytes store excess energy and can eventually result in metabolic diseases like obesity, while brown adipocytes dissolve this stored energy into heat.
To uncover a therapy that could stimulate the production of brown adipocytes, the researchers combed through Calibr’s ReFRAME drug-repurposing collection—a library of approximately 14,000 known drug compounds that have been approved by the FDA for other diseases or have been extensively tested for human safety.
This is how they uncovered zafirlukast, an FDA-approved drug used for treating asthma. They found zafirlukast could turn adipocyte precursor cells into predominantly brown adipocytes, as well as convert white adipocytes into brown adipocytes.
While an encouraging find, zafirlukast is toxic when administered at higher doses, and it wasn’t entirely clear how zafirlukast was converting the fat cells. This is when the researchers partnered with Siuzdak and his team of metabolite experts.
They designed a novel set of experiments, known as drug-initiated activity metabolomics (DIAM) screening, to search through thousands of molecules and identify specific metabolites. After reducing 30,000 metabolic features to just 17 metabolites, they found myristoylglycine—an endogenous metabolite that prompted the creation of brown adipocytes, without harming the cell. Of the thousands of metabolic features measured in the analysis, only myristoylglycine had this special characteristic.
“Our findings illustrate what happens when an analytical chemistry team and a drug discovery group closely collaborate with each other,” says co-senior author Kristen Johnson, director in Translational Drug Discovery Research at Calibr.

BROWN FAT
Finding drugs that fix fat cells

Enrique Saez, PhD
Professor of Molecular Medicine
When Enrique Saez was in graduate school during the 1990s, the field of obesity research was rocked by two discoveries: leptin, a hormone made by fat cells that regulates appetite, and a protein that regulates the expression of genes involved in fat regulation and storage. Yet researchers routinely threw away the fat tissue they collected because they assumed it had little value.
Saez wondered why there wasn’t more interest in the biology of fat itself. “At the time, obesity-linked diabetes was already a major disease, so I thought, ‘Why not focus on the defects in the fat tissue that lead to diabetes?’” he says. “I was curious if we could discover new mechanisms that could restore its proper functioning.”
So began Saez’s fascination with fat cells and how they become dysregulated. Researchers in the field had found that gaining a large amount of weight can cause fatty acids known as lipids to accumulate inside fat cells. As these cells balloon, the lipids eventually spill out and get deposited in other organs—causing widespread metabolic problems and leading to diseases such as type 2 diabetes. Rather than focus on developing diabetes drugs that treated the symptoms by targeting the pancreas or liver, for example, his lab has identified several drug compounds that get to the root cause of the problem: They fix the abnormalities in fat cells and restore their ability to retain lipids. “We wanted to discover new biology that could be leveraged to treat metabolic disease,” Saez says.
In their next breakthrough, Saez and his team found a signaling protein that activated the whole process. In research that was published in Nature in 2019, they showed that the protein PGRMC2, which is abundant in so-called brown fat that helps regulate body temperature, protects heme, a natural molecule that’s involved in many cellular functions, such as energy production in mitochondria and circadian rhythms. They learned that PGRMC2 was a “chaperone” protein that delivered heme to other proteins throughout the cell that need heme to function. Activating this pathway using an experimental drug improved metabolic health for the obese and diabetic mice in the study: They became more glucose tolerant and sensitive to insulin and had less fat in their livers and inflammation in their fat tissue.
In the future, Saez wants to explore whether this protein plays a role in other diseases, such as the genetic disease hemochromatosis, a disorder of heme and iron accumulation in the liver. (His college roommate was affected by it and had to get regular bloodletting procedures.) Eventually, he hopes to find a pharmaceutical partner to develop a therapy. “This is important research because the incidence of metabolic diseases is increasing around the world,” says Saez. “What we’re trying to do is use chemical tools to discover new mechanisms to treat them and improve human health.”

Discovering a new pathway to treat metabolic disease
Luke Wiseman, PhD
Professor of Molecular Medicine
As the rate of metabolic syndrome soars globally, Luke Wiseman wanted to find a new approach to treat this group of conditions that increases one’s risk of heart disease, stroke and type 2 diabetes. The need couldn’t be greater: For those patients who don’t follow the most-prescribed advice to improve their condition through lifestyle changes, such as diet and exercise, healthcare providers have few choices but to offer piecemeal interventions, such as medications to control blood pressure, cholesterol or blood sugar levels.
Specifically, Wiseman wanted to explore a cellular signaling network known as the unfolded protein response to see if it could lead to a more comprehensive treatment. Over the past decade, Wiseman has studied how stress—including everything from pollution, temperature, aging and unhealthy food choices—causes unfolded proteins to accumulate within the cell, impacting its ability to function and contributing to disease onset and progression.
Making this scenario even more intriguing was the fact that a certain aspect of the unfolded protein response, which is regulated by the protein IRE1, could protect cells against metabolic dysfunction. However, finding the sweet spot was tricky, as overactivation of this pathway could cause inflammation and cell death. “I was interested in asking, ‘How could we activate the good parts of this pathway without triggering the bad ones?’” says Wiseman. More importantly: Could they find a drug to do it?
Working with celebrated Scripps Research chemist Jeffery Kelly, the Lita Annenberg Hazen Professor of Chemistry, they screened more than 650,000 small molecules and decided to test an experimental compound called IXA4, which selectively activated the good parts of IRE1 signaling. Then Wiseman reached out to his colleague, metabolic disease expert Enrique Saez (also featured in this article), to help run an experiment that would illuminate if the drug improved metabolic function in obese mice.
During the study, the team discovered that the IRE1 activator drug reduced the rodents’ glucose production, cleared out fatty buildup in the liver and improved insulin regulation in the pancreas—protecting the animals from the obesity-related metabolic changes associated with diseases including type 2 diabetes. The results were published last year in the journal Nature Communications.
“The potential implications are enormous,” says Wiseman. “What’s exciting is that we’ve discovered how to give cells the tools they need to better respond to stress and eventually prevent many diseases.” Next, the team is planning to investigate whether the drug could help patients with types of fatty liver disease like nonalcoholic steatohepatitis (or NASH) that have no treatment options. This research also opens the door to develop new approaches for other types of disease in the future, including neurodegenerative diseases like Alzheimer’s, protein misfolding diseases and ischemic disorders like stroke and heart attacks.
“This is just the tip of the iceberg,” he says.