The retina is an extension of the central nervous system, and so far, nearly impossible to transplant or regenerate. But Associate Professor Anne Hanneken, MD, is working to change that. For decades she has worked days and nights, balancing the care of patients with retinal diseases at Scripps Memorial Hospital La Jolla while leading groundbreaking ocular research at her Scripps Research lab. Her work has led to unprecedented discoveries in the fields of eye science, including a way to revive the human eye after death, and promising potential treatments for age-related macular degeneration.
Scripps Research Magazine sat down to talk with Hanneken about her path to science and the pursuit of her ultimate goals: making progress in transplanting retina tissue, as well as curing blindness and debilitating eye disease.
When did you first realize you wanted to become a scientist?
I’m the oldest of seven siblings and it seems like I was born interested in science. My father was the chairman of mathematics at Marquette University in Milwaukee, Wis., and we always had academic discussions around the kitchen table. He was very much a basic mathematician while I was very much an applied scientist. We used to have friendly discussions about which is more valuable. He ended up winning every time because the basic science is always necessary for any applied science.
What drew you to eye research?
I first became interested in eye research during one of my jobs in an ophthalmology research lab at the Medical College of Wisconsin, where they were developing a new field called vitreoretinal surgery to restore sight to blind patients with diabetes. MCW was one of the world’s leading programs, and this experience left me with a strong interest in pursuing this career after medical school. While at MCW, I learned more about the cause of diabetic blindness, a process called ocular angiogenesis—the formation of abnormal blood vessels—which ultimately led me to Dr. Judah Folkman’s lab in Boston and then to the Johns Hopkins Wilmer Eye Institute for my residency, where I continued this line of work.
Since becoming a clinician, I have seen firsthand how losing your sight dramatically changes people’s lives. When you suddenly lose your central vision, you can’t live independently any longer. This experience is devastating for most people. You might not realize that one of the most difficult transitions for people is the loss of their driver’s license, which represents their sense of independence and freedom. I’ve had patients take big risks to keep driving and then become very depressed if they are unsuccessful. Many of these people suffer from ocular conditions that lack adequate treatments, which is our motivation to pursue innovative research.
What was your path to Scripps Research?
After finishing my vitreoretinal fellowship at Duke University, I moved to La Jolla, Calif., to work with world-renowned researcher Roger Guillemin who had won the Nobel Prize in Physiology or Medicine. I spent five years as a postdoc in his lab at the Whittier Institute for Diabetes and Endocrinology. During that time, he used to come into my office at the end of the day and tell me that in my lifetime we would be doing eye transplants. Back then, I wanted to tell him it was a crazy idea. But you can’t really tell a Nobel laureate their ideas are crazy. So, I quietly listened and thought about it over the years. It turns out he was ahead of his time. He introduced me to Dr. Alberto Aguirre in Montreal whose lab was working on optic nerve regeneration and encouraged me to work in that area.
After Whittier, I joined Scripps Research with several other basic scientists who moved over in a large group. I have been here since 1995 and I love it. I chose Scripps Research because I didn’t want to be in a clinical department where everyone thought the same way—I wanted to be in an environment where I would be surrounded by the world’s best chemists and biologists so that we could collaborate across fields to tackle some of the major and complex problems in medicine.
How do you balance running a successful lab and treating patients in the clinic?
It’s a very difficult thing to balance both a clinic and lab. At Hopkins, I did research at night and on the weekends, and when I left, I promised myself that at one time in my life I would do research when the sun was shining. Now, I still do some research at night and on weekends—the organ donor work taking place in the middle of the night—but much of the research time is when the sun is shining. There’s not a lot of support to pursue both clinical work and basic science. When I interviewed for academic positions following my fellowship at Duke, I found most clinical chairmen did not want their clinicians doing much research because it reduces their clinical revenue. I thought there were much better opportunities in a research institute where you could find scientists with other areas of expertise that you can collaborate with and ask questions that are important in your field.
Are you working on any collaborations now?
We’ve been working closely with Dr. Arthur Olson at Scripps Research using computational modeling and virtual screening to identify binding partners that modulate vision. One of our most exciting projects relates to the recent discovery of binding sites on rod and cone opsins in the human retina, which are the light receptors in the human eye that absorb dim as well as colored lights.
Traditionally, these sensitive light receptors have been thought to have only one binding partner (a vitamin A derivative that binds to the receptor). But we discovered a group of molecules that affected vision independent of light. We were able to use computational modeling to predict the location of these binding sites and gather evidence which explains chemically how these molecules change the conformation of opsin from one structure to another.
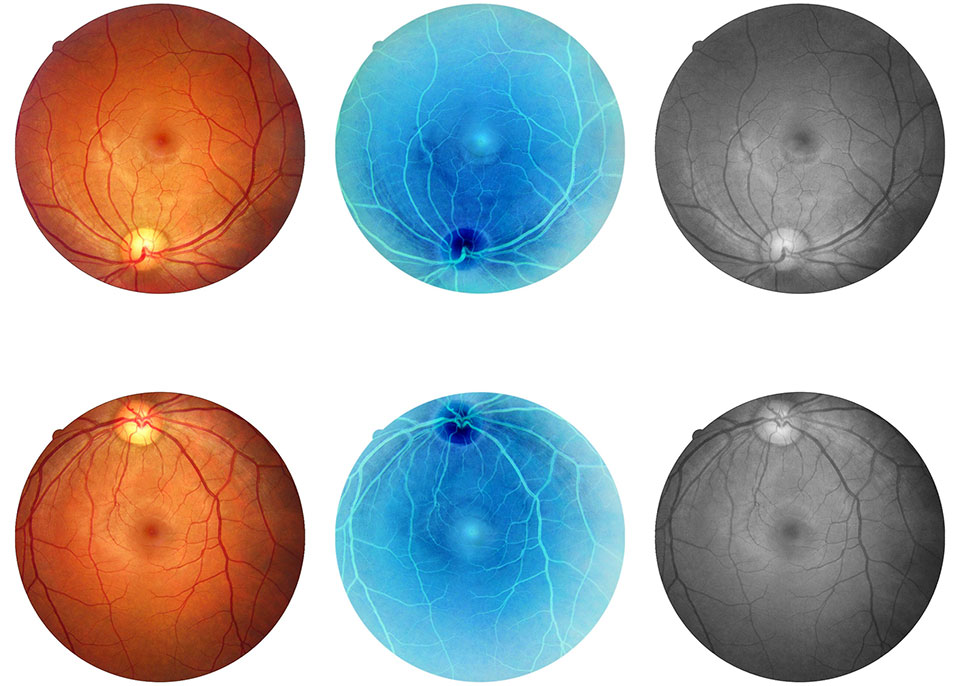
Our recent goal was to test these binding partners in the human retina to find out whether they would impact visual chemistry in a human eye in the same way they seem to impact visual chemistry in our lab assays. This goal required that we recover functional human retinas from autopsy eyes. This work ultimately led to our major 2022 paper showing that the eye can be revived after death and the electrical activity can be restored in the central vision.
Ultimately, we’re hoping these small molecules could become a treatment for patients with age-related macular degeneration. Patients who have this condition start out having difficulty transitioning from light to dark—many cannot see at all in a dark room—and no one knows exactly what causes this abnormality. We think the current dogma is false and that the problem lies elsewhere. Our research shows that these molecules can improve dark adaptation by increasing the speed of visual chemistry. The next step is to test these molecules in functional human retinas and find out whether they can overcome these defects in visual chemistry. It is not sufficient to perform these studies in animals because animal models do not develop the type of macular degeneration that is seen in humans. Evaluating the biological effect of these allosteric molecules in diseased human retinas is one of the reasons we needed to revive human donor eyes.
What did you discover in that landmark 2022 Nature paper?
Together with collaborators at the University of Utah and the Salk Institute, we made the surprising discovery that the human eye can be removed from the body even hours after death and the function of the light-sensing cells in the central vision can be revived. Specifically, we focused on the human retina, a highly sensitive system that is prone to deterioration due to inherited gene mutations or age-related conditions, including diabetes and age-related macular degeneration. We were essentially able to get the cells to ‘wake up’ and talk to each other after death. We did this by removing the organ and restoring oxygen and a normal acid-alkaline (pH) balance, while tracking its activity using a method called electroretinography (ERG).
We’re hoping that this new ability to revive the central human retina and study it directly in the laboratory will lead to a much better understanding of vision and better care for the millions of patients with retinal diseases.
Does this discovery have implications for the biology of death?
Our findings made me think more about the definition of brain death. If you can restore neuronal communication and trans-synaptic communication within an hour after circulatory death, it makes me wonder whether brain death might be reversible for a limited time after cardiac death. We might think about brain death as occurring 60 minutes after circulatory death, a time after which we couldn’t recover trans-synaptic communication. That’s what we found in the Nature paper: 60 minutes seemed to be the magic number. You can revive nerve tissue within that time and restore trans-synaptic communications. This brings up a lot of questions that are worth exploring.
“Our findings made me think more about the definition of brain death. If you can restore neuronal communication and trans-synaptic communication within an hour after circulatory death, it makes me wonder whether brain death might be reversible for a limited time after cardiac death.”
You mentioned your interest in transplantation as well— why is it so difficult to transplant the eye from a donor into a patient?
You can transplant a heart, lung, kidney and other organs and they will function well in the host. But transplanting organs or tissues from the central nervous system, such as the eye, is a different challenge altogether because nerves need to integrate into an environment that is not friendly to nerve regeneration.
It’s difficult to take a patch of the retina and try to get it to integrate into a collection of nerves. There is no current medication we can use to stimulate synaptic regeneration or neuronal integration. Axonal regeneration has been a big obstacle after spinal cord injury. Axonal regeneration also limits the rehabilitation of patients who have glaucoma or other eye diseases that require retinal ganglia cells to regenerate axons from the retina to the brain. That’s a major challenge.
What do you do when you take a break—you’ve been involved with sports in the past, is that right?
I enjoy skiing and running, as well as cooking and spending time with my family. Fun fact: in college I played on the men’s tennis team because they didn’t have a women’s team. Eventually I organized the first women’s tennis team at Marquette and was recently awarded the Alumnus of the Year award for jumpstarting the women’s athletic program there. That project was complex, just like basic research, but it was very exciting to have a positive impact.
How has philanthropy affected your research?
What could be more important than philanthropy? Much of my retinal transplant work would not have been funded through traditional means, as it’s too out-of-the-box/high-risk, high-reward research. Donors are eager to see this work extended. For example, we’re aiming to prolong the lifespan of the revived human eyes to study the transplantable window, as well as reverse the effects of hypoxia after death. Overcoming the effects of hypoxia on nerve tissue could have a major impact on strokes and neurodegenerative diseases as well.
Donor support also helps to gather the best and brightest collaborators. For example, for some of this work, you need a vision scientist, electrophysiologist, a clinician, an eye bank, etc.