Targeted cancer treatments based on Scripps Research antibodies head to clinical trials
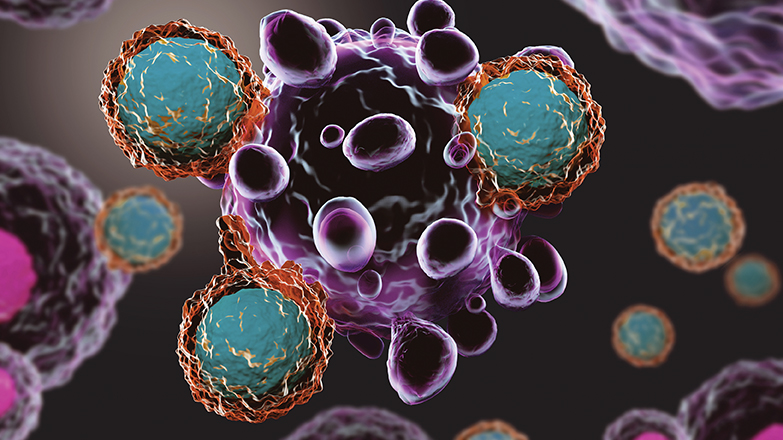
Antibody drugs are like medicines tagged with a GPS system: they go only exactly where they’re told. That should make them an ideal homing system for finding and destroying cancer tumors, says Scripps Research biochemist Christoph Rader, PhD, in Florida. But creating such a system hasn’t been so easy.
That’s because cancer grows from our own cells, so for the most part they look friendly to our immune system. For an antibody drug to work, it has to be sent to a unique “address” that’s not shared with any healthy cells.
“Antibodies are only as good as their targets,” Rader says. “It’s all about finding subtle differences on the surface of cancer cells.”
—Christoph Rader, PhD
Professor, Scripps Research

And that’s what Rader has done. At Rader’s previous lab at the National Cancer Institute in Maryland, he and his team found that a mysterious gene known as ROR1 was showing up on the surface of certain leukemia and lymphoma cells but not on healthy cells. Other researchers subsequently discovered the gene on breast and lung cancer cells, as well as other solid tumors.
Today, 13 years since Rader published his discovery, two antibodies developed in his labs at NCI and Scripps Research are now in clinical trials. Trial sites include the Fred Hutchinson Cancer Research Center in Seattle and the MD Anderson Cancer Center in Houston.
“We use phage display, a technology developed many years ago at Scripps Research, to generate rabbit antibodies that zoom in on human targets with exceptional precision,” says Rader. “But in the case of ROR1, precision alone was not enough. We also needed to empower the antibodies with the ability to kill cancer cells quickly and efficiently.”
For this, Rader teamed with collaborators. One used ROR1-targeting antibodies to build a powerful cancer immunotherapy known as chimeric antigen receptor T cells, or CAR-Ts. Another converted the antibodies to so-called “antibody-drug conjugates” which deliver chemotherapy to cancer cells without harming healthy cells.
The advancements grabbed the attention of the pharmaceutical industry. Two small biotech companies focused on ROR1-targeting antibody drugs—one of which was based on a rabbit antibody from Rader’s Scripps Research lab—were recently acquired in major big pharma deals.
Rader shares credit with staff scientist Haiyong Peng, PhD, who “single-handedly designed, built and selected a library of 10 billion rabbit antibodies to find this lead,” Rader says. Peng’s library also turned out to be a gold mine for other promising cancer treatments now in development.
As for cancer treatments targeting ROR1, the future is getting brighter every day, he says. “Being picked up by pharmaceutical partners allows clinical trials to kick into high gear,” Rader says. “We’re proud to have contributed to this endeavor.”