Clinical trials and clinical research studies are a crucial part of bringing medical innovations from the bench to the bedside. Traditional clinic-based trials, however, have several limitations. Trial participation is limited to those with access to the trial clinic, as well as the ability to take time off work to attend in-person clinic visits. Such barriers mean that scientists often struggle to meet study enrollment goals and have resulted in a lack of diversity across demographics in study populations.
Additionally, data gathered during a handful of clinic visits provides an incomplete, episodic picture of a person’s response to the intervention being studied.
Scientists at the Scripps Research Digital Trials Center are addressing these challenges with the help of digital technologies such as wearable sensors, smartwatches, fitness trackers and mobile applications. These technologies allow scientists to recruit, monitor and communicate with study participants remotely. By designing trials around the participant instead of a study site, trials can be more inclusive and scale to enroll large numbers of participants across sweeping geographical areas.
Advances in digital health technologies also allow for continuous monitoring of behavioral and physiological metrics, such as heart rate, blood sugar, activity and sleep. Being able to collect longitudinal data on study participants gives scientists much more detailed insights into how their bodies are responding to any given intervention, enabling a more individualized approach to medicine.
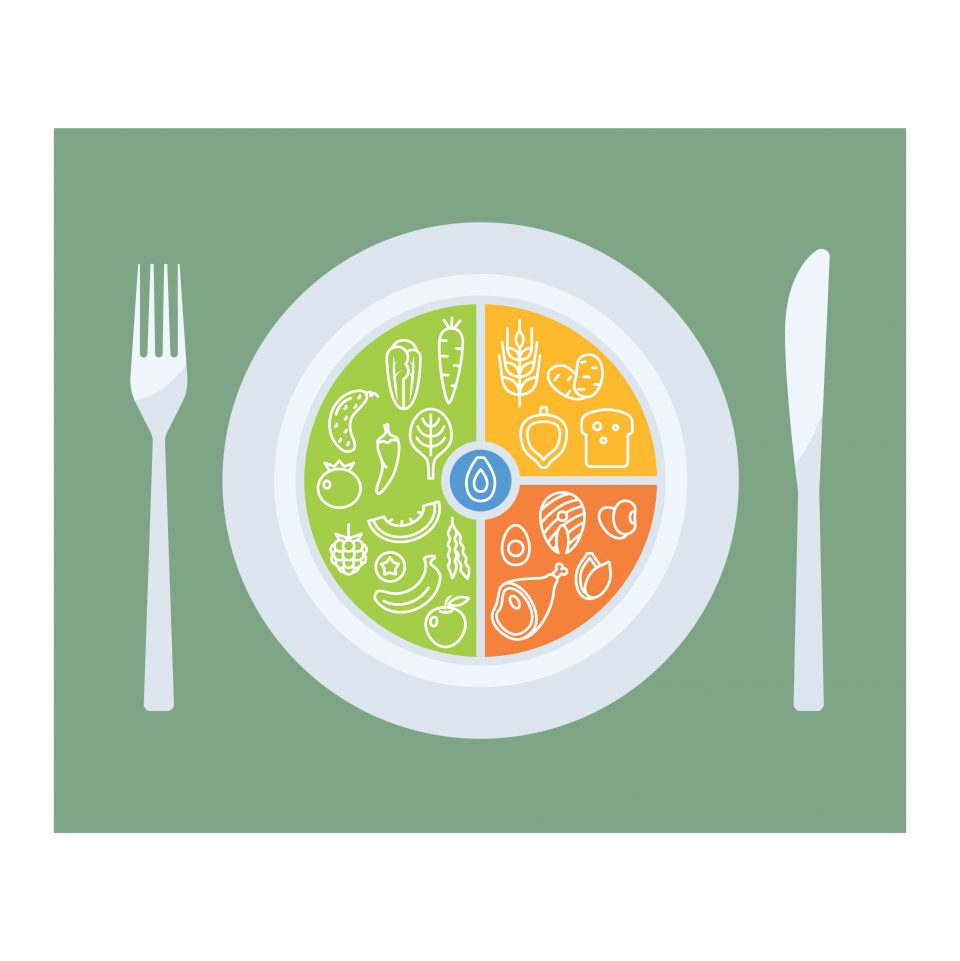
Scientists at the Digital Trials Center are pioneers in this site-less clinical trial model and are applying it to the study of a broad spectrum of disease areas and conditions, from COVID-19 and precision nutrition to maternal health and sleep. Most recently, the team launched the PRediction Of Glycemic RESponse Study, or PROGRESS. To understand the different ways our bodies respond to food intake, and how those responses impact our blood sugar, referred to as glucose levels, PROGRESS will gather data from 1000 participants using a host of digital devices and mobile apps. The study may help guide better nutritional health and provide new insights into factors that contribute to type 2 diabetes.
Visit progress.scripps.edu to learn more.
PROGRESS Study Participant Journey
Step 1
Learn about study
A prospective participant learns about PROGRESS through a digital marketing campaign—either on social media (the neighborhood app “Nextdoor”) or via an email from a participating health provider organization.

Step 2
Download MyDataHelps™ app
The prospective participant then installs the MyDataHelps app on their mobile device.

Step 3
Review of eligibility criteria & e-consent
To enroll as a study participant, a person must review the eligibility criteria and go through the e-consent process. This is done via the study app.
Congratulations, you are now a participant!
Step 4
Connect & share electronic health record data
Once enrolled, the participant is asked to share their electronic health records by connecting the app with Apple Health Records (for IOS users) or directly with the patient portal used by their health provider.

Step 5
Complete surveys
The participant is prompted by the app to answer several surveys on their medical history, lifestyle, stress and other health related topics.

Step 6
Collect samples
A “BioKit” is mailed to the participant to collect blood, saliva and stool samples. Participants will be prompted to walk through the collection process by watching video tutorials within the app. A study coordinator will be available to answer any questions.

The blood sample, collected by the participant with a single-use, home micro-puncture device, is used to measure the amount of glucose, or sugar, in the blood.
A saliva sample will be collected for genomic sequencing. Genomic information will allow scientists to study the functions of genes that may influence glycemic response—the fluctuations in blood sugar levels after food is consumed.
A stool sample, collected with a gut microbiome kit, is used to study the impact billions of bacteria and other microorganisms in the gastrointestinal system have on functions like digestion and metabolism.
The samples are mailed by the participant to processing laboratories and the data is analyzed by scientists at Scripps Research.
Step 7
Complete additional survey
The participant is invited to answer an additional survey on food intake via the study app.
Step 8
Participate in 10-day study period
A “GlucoKit” is sent to the participant which includes a wearable continuous glucose monitor sensor that will gather data on fluctuations to the participant’s blood sugar levels.

The participant will be asked to connect their fitness tracker to the MyDataHelps study app. This will allow the collection of physiological and behavioral metrics like blood pressure, heart rate, sleep and activity, during a 10-day study period.
Two meal replacement bars are provided for two breakfasts after an optional 8 hour overnight fast. This is a controlled meal and will help researchers understand more about glucose elevation with the provided meal bar.
During this time, participants will also record all their meals using an app-based smart photo food journal. A study coordinator will be available to assist the participant during the 10-day study period.
Step 9
Return of personal and study information
Personalized information gathered throughout the duration of the study, whether it be individual glycemic responses to recorded meals or ancestral genomic information, is communicated back to the participant when available. When ready, participants will be able to access a report with their individual results in-app or via email.
Step 10
3-year follow-up
Participants will periodically be asked to answer questions about current health and medical history over a 3-year follow-up period.
To learn more: progress.scripps.edu
The study includes an incentive point system intended to motivate participants as they advance through the study activities. More time-consuming tasks, such as biosample collections will earn the participant more points than easy activities like responding to surveys.
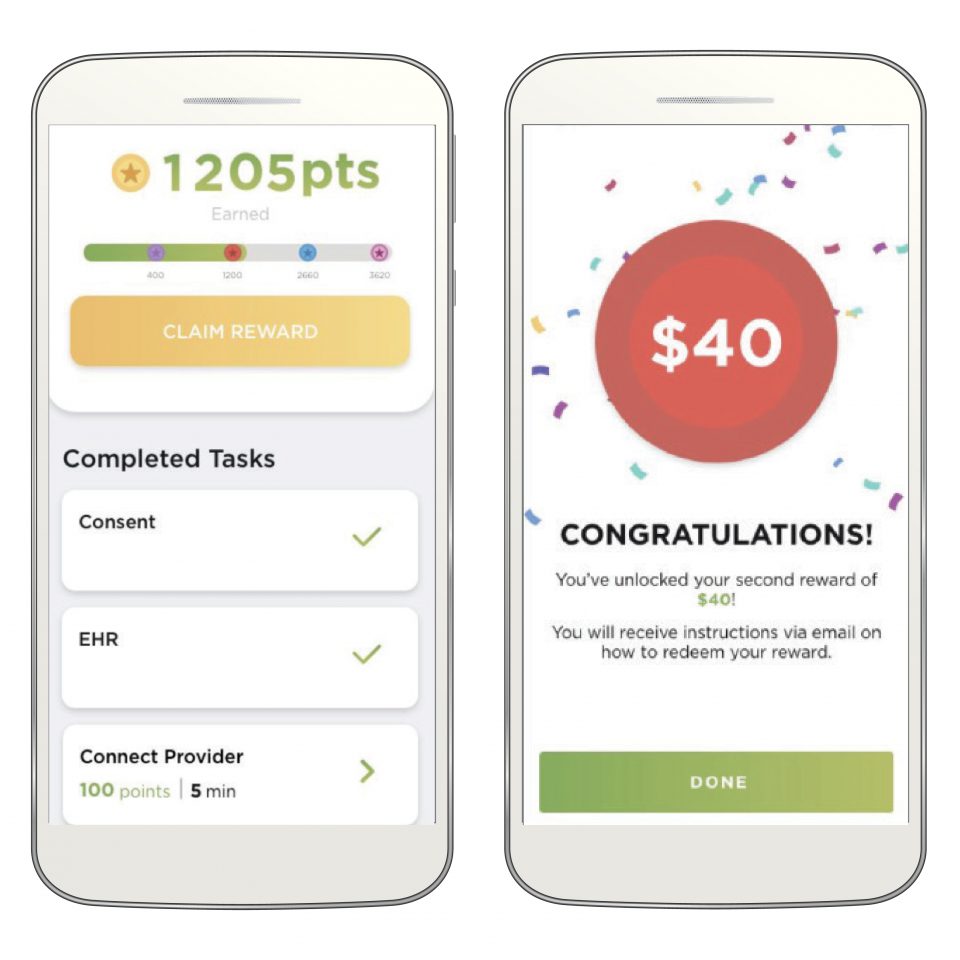
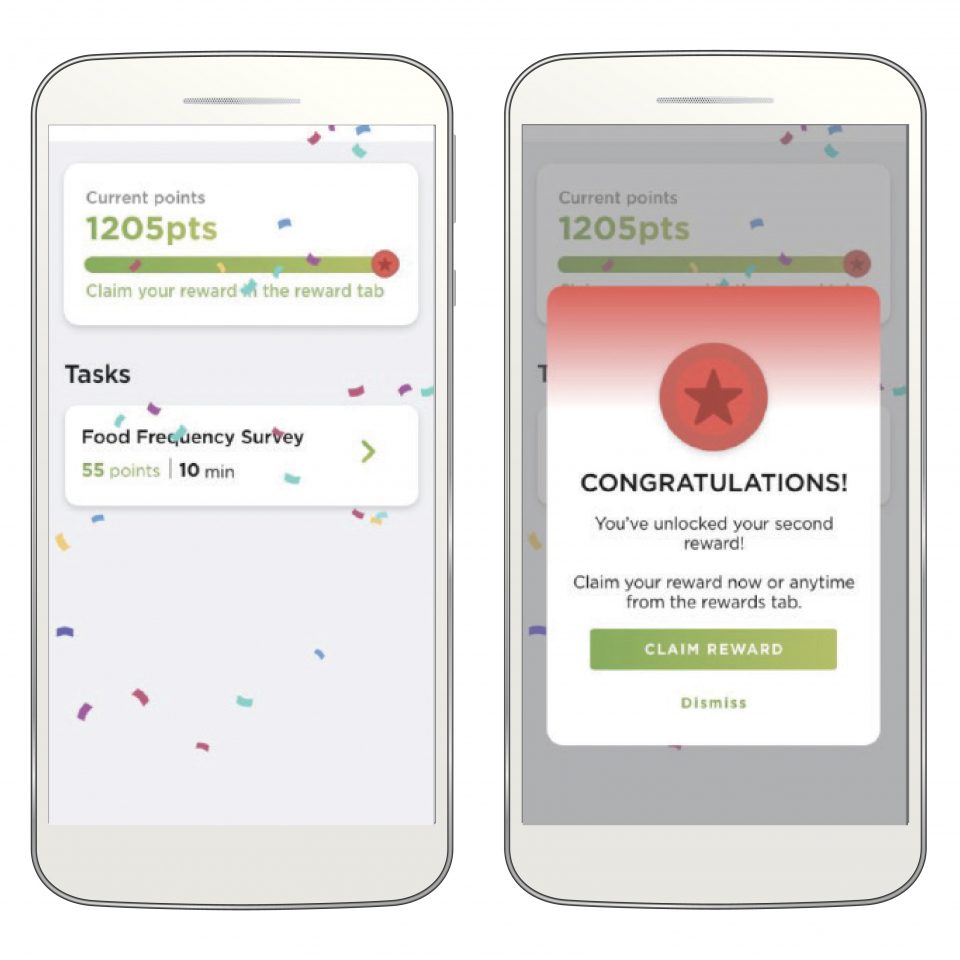
Points will translate into rewards which the participant can redeem through electronic gift cards.
Participants will also be able to keep the fitness tracker provided to them as a thank you for participating in the study.